Internal Medicine Residency
Our internal medicine residency program provides an excellent clinical education while creating integral members of our medical community.
Internal Medicine Residency
Welcome to Our Program!

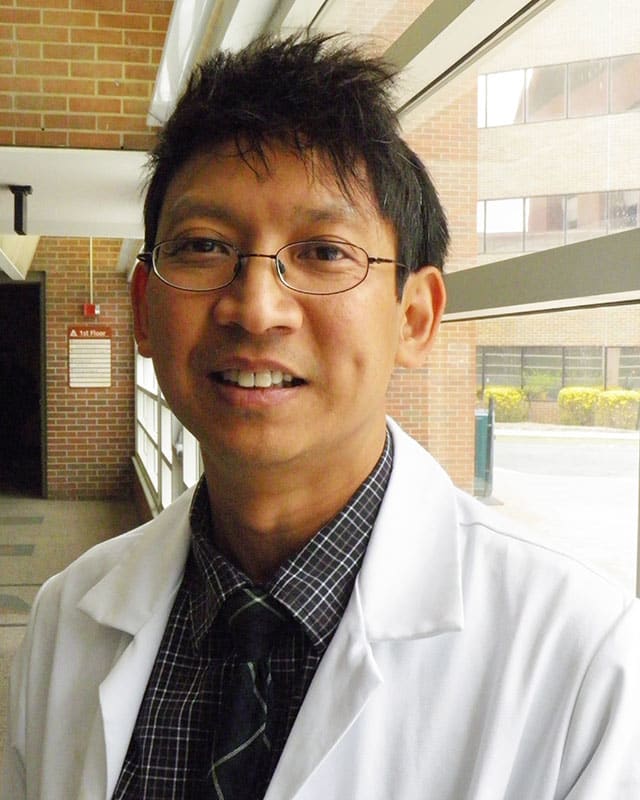
Welcome from the Program Director
Welcome to the website for the Internal Medicine Residency Program at Berkshire Medical Center and thank you for your interest in our training program!
As a residency, we are committed to providing exceptional clinical education to produce highly qualified future primary care, hospitalist, and subspecialist physicians. Our residency leadership is committed to collaborating with our residents to provide a community atmosphere to support growth and independence throughout training.
Our residents work primarily in the active academic environment at Berkshire Medical Center, teaching and supervising medical students from multiple teaching affiliates – including the University of Massachusetts, the University of New England, and Boston University Medical Schools. Residents at BMC are also an integral part of the local medical community beyond the hospital, and work to care for patients throughout Berkshire County at a variety of outlying clinics and health centers. We have outstanding clinical educators amongst our teaching faculty, a strong tradition of clinical research, and innovative ways of creating career-specific training. We are fortunate to be able to live and work in the beauty of Berkshire County and proud that many of the current internists and subspecialists in our community previously trained in our program. Most notably, we are proud of our ability to provide high-quality patient care and our educational strength, as reflected by Berkshire Medical Center’s designation as one of the Top 50 Teaching Hospitals in the US in 2020 & 2021 by the Leapfrog group!
*New for the March 2026 Match season* We are opening a Primary Care Focus Track, which will add 2 additional positions within our program (2 residents to start in July, 2026) for incoming trainees particularly interested in possible future outpatient-based practice. See the Primary Care Track section of our site below for further details.
As you review this site, I hope that you will appreciate the unique opportunity our program provides to receive excellent clinical education (including both the art and science of medicine), while becoming an integral part of a medical community.
Warmly,
Steven Lamontagne, MD
Program Director, Internal Medicine Residency
Medical Education Affiliates



Program Information
Program at a Glance
Categorical Positions: 13/year
Preliminary Positions: 5/year
Total Program Residents: 44 currently*
Chief Residents: 2/year
Founding Date for Residency Program: 1961
*Adding 2 designated Primary Care Track positions/year starting in July 2026 – with ultimate program size increasing to 50 trainees.
Schedule Summary
We are proud of the educational content of our training program, and the scholarly work that our residents produce.
Typical yearly schedule is as follows:
(each block consists of a 4-week rotation)
| PGY-1 | |
| Ward Medicine | 5 |
| Critical Care Medicine | 2 |
| Subspecialty Electives | 4 |
| Ambulatory Medicine | 1 |
| Night Medicine | 1 |
| PGY-2 | |
| Ward Medicine | 3 |
| Critical Care Medicine | 2 |
| Subspecialty Electives (including Quality Improvement Rotation, & Addiction Medicine experience) | 4 |
| Ambulatory Medicine | 1 |
| Night Medicine | 1 |
| Consult Medicine | 1 |
| Evening Float | 1 |
| PGY-3 | |
| Ward Medicine | 3 |
| Critical Care Medicine | 2 |
| Subspecialty Electives | 6 |
| Ambulatory Medicine | 1 |
| Consult Medicine | 1 |
General Benefits
Medflex:
Berkshire Medical Center’s flexible benefit program includes health insurance options, dental insurance options, basic life insurance, supplemental life insurance, long and/or short term disability insurance, health care and dependent care spending accounts on a tax free basis, and spouse and child term life insurance on an after-tax basis. The flexible benefit program provides dollars provided by BMC to be applied toward the purchase of benefits on a pre-tax basis, or a lesser sum to be taken as taxable cash if your spouse provides health insurance for you from another source. The dollars, if utilized for health insurance, include 90% of the cost of individual coverage or 75% of family coverage based on Network Blue New England. Benefit dollars are provided to partially cover dental insurance premiums, and to fully cover the cost of the long-term disability (50% option).
– Health Care Spending Accounts allow you to contribute pre-tax money weekly for health care expenses not covered by health insurance plans. It can add tax savings to the protection you receive from our medical and dental plans.
– Dependent Care Spending Accounts let you pay your dependent care fees on a pre-tax basis, as long as the care makes it possible for you to work.
Basic Life Insurance:
A term life insurance is provided, paid in full by BMC covering one times your annual salary, effective upon date of hire.
Uniforms:
White coats and scrubs and laundry of these garments will be provided.
Professional Liability:
Liability insurance is provided for house officers free-of-charge during the term of the contract. Coverage pertains to in-hospital activities only. Limits are stated in contract between BMC and the Berkshire Insurance Company. Tail coverage is included in this policy.
Registration Fees:
Registration fees for temporary licenses are covered for house officers who are not permanently licensed in the Commonwealth of Massachusetts.
Vacations:
Each house officer is entitled to four (4) weeks of vacation with pay each year.
Education Benefits
Each year, the following allowances are available for educational resources (online learning resources, books, journals, other educational resources). Allowances may not be carried over from one year to the next, and are not able to be used for USMLE Step 3 or Board Examination registration fees.
- PGY-1 $1500 per year
- PGY-2 $1500 per year
- PGY-3 $1500 per year
A complete Board Review Course is provided on-site in the PGY-3 year for Internal Medicine residents.
Supporting Wellness
The ongoing Wellness of our trainees within our program is a major priority for us! We recognize that as physicians we will only be able to excel in our clinical practice when we are supported and focused/content with our life and work overall.
We at BMC are proud to have numerous programs & supports in place to support our residents throughout training, including:
- Our Medicine Residency Wellness Committee
- Bi-Annual Wellness screenings – for all residents
- A robust Institutional Wellness Department (promotes/sponsors regular out-of-work activities)
- Holiday Scheduling (with lighter resident staffing) for Major Holidays
- Resident Appreciation Day Celebration
- With a shortened workday allowing for an afternoon of rest/camaraderie/socialization in June each year
- Free access for all residents to the TalkSpace App (virtual counselling service)
- On-Site/Confidential In-Person counselling for all employees
- Wellness afternoons: All residents on a Ward Medicine Rotation are able to take an afternoon completely off clinical work once during each 4-week rotation
- A yearly Team-Building Retreat for PGY1s mid-internship
Fun Outside of Work
Applying to the Internal Medicine Residency Programs
The Berkshire Health System participates in the Electronic Residency Application Service (ERAS).
- Applicants’ ERAS applications are reviewed on a rolling basis from the date on which they become complete.
- Regarding Program Signaling: Our program will preferentially review applications from those who have signaled our program – BUT we will also review applications for applicants who do not signal us.
- To complete your ERAS you will need:
- Personal Statement
- Dean’s Letter
- Transcript
- 3 letters of recommendation (minimum)
- USMLE or COMLEX Level 1 & 2 scores
- Completed applications are reviewed and qualified applicants are identified based on academic performance, Exam scores, letters of recommendation and clinical experience.
Applications are accepted through the Electronic Residency Application System (ERAS).
Apply Today through ERAS SystemNRMP Program Codes:
- Traditional Track Code: 1281140C0
- Primary Care Track Code: 1281140C1
- Preliminary Track Code: 1281140P0
Visa Sponsorship:
- For Categorical residency applicants: H1 Visas are sponsored
- For Preliminary year applicants: J1 Visas are sponsored
Interviewing for our Programs
We are planning to conduct all interviews virtually (via computer) for the 2025-2026 season.
Interviews will be offered & scheduled on a rolling basis – with our interview season beginning in Late October 2025 and concluding in January 2026.
Regarding Program Signaling: Our program will preferentially review applications from those who have signaled our program – BUT we will also review applications for applicants who do not signal us.
Primary Care Track
New for 2025-2026
Our program is excited to be opening a dedicated Primary Care Track – aiming to enroll two additional residents each year (with our first cohort to start training in July 2026) who are particularly interested in future primary care practice. Residents in this track will be fully integrated within our tight-knit general internal medicine training program (for inpatient and subspecialty medicine learning) and gain the benefit of comprehensive outpatient-based education (including close faculty mentorship and extensive training in a real-world primary care setting) to allow graduates to seamlessly transition to highly efficient and expert-level practice in ambulatory medicine.
Primary Care Track at a Glance:
In addition to joining in the standard educational elements of our current Internal Medicine program (Ward Medicine, Critical Care Medicine, Subspecialty Rotations), our Primary Care Track Trainees will have unique outpatient-focused learning opportunities, including:
Structured Ambulatory Blocks: Residents rotate through their Longitudinal Clinic in dedicated outpatient-focused blocks.
Longitudinal Continuity Clinic: Weekly clinic sessions across all three years of training with close faculty mentorship, and the ability to be a Primary Care Physician to a dedicated group of patients. We aim to utilize our institutional-affiliated practices with a longstanding history of teaching excellence for these rotations.
Ambulatory Expertise Rotation: Subspecialty exposure in the fields that most closely overlap with primary care, including Urology, Behavioral Health, ENT, and Dermatology.
Schedule Summary:
Each block consists of a 4-week rotation:
| PGY-1 | Blocks |
| Ward Medicine | 4 |
| Critical Care Medicine | 2 |
| Subspecialty Electives | 3.5 |
| Primary Care Expertise Rotation: A combination of outpatient Dermatology, Ophthalmology, Sleep Medicine, Urology, Behavioral Health Medicine | 1 |
| Ambulatory Medicine | 2 |
| Night Medicine | 0.5 (2 weeks) |
| PGY-2 | Schedule Under Development |
| PGY-3 | Schedule Under Development |
Applying to the Primary Care Track:
Applying for the Primary Care Track is via ERAS. Designate your application for the Primary Care Track through NRMP Code: 1281140C1
Our Berkshire County Primary Care Residency Alumni
Build your career & your life in a place that supports both.



Lenox Family Health

Hillcrest Family Health

Lenox Family Health
Preliminary Medicine Internship
The Internal Medicine Residency accepts 5 trainees per year for a one-year Preliminary Medicine program.
The academic schedule is very similar to that of a Categorical Intern, with:
- 6-7 blocks of Inpatient Ward Medicine
- 1 block of Critical Care Medicine
- 4-5 Subspecialty Rotations
Our recent Preliminary graduates have moved on to outstanding training positions, including:
Neurology:
- Baylor Medical Center
- Drexel Medical Center
- Tulane Medical Center
- University of Massachusetts
- University of Maryland
Physical Medicine & Rehabilitation:
- Case Western Reserve Medical Center
- Cleveland Clinic Medical Center
- Eastern Virginia Medical Center
- New York University
- Northwestern Medical Center
- Penn State Medical Center
- Sunrise Health Center
- University of Wisconsin Medical Center
Radiology:
- Baystate Medical Center
- Lahey Clinic
- Massachusetts General Hospital
- Penn State Medical Center
- St Louis University Medical Center
- St Vincent’s Hospital
- SUNY – Downstate Medical Center
- Texas Tech Medical Center
- University of Texas Medical Branch
- Virginia Commonwealth Medical Center
Anesthesiology:
- Rutgers Medical Center Opthalmology
- Stanford University Medical Center
- Tufts Medical Center Dermatology
- University of Connecticut
Dermatology:
- Rutgers Medical Center
Ophthalmology:
- Stanford University Medical Center
Osteopathic Focus Track
Background & Community of Osteopathic Learning:
Berkshire Medical Center (BMC) is a major teaching affiliate of the University of New England College of Osteopathic Medicine (UNECOM) and serves as a primary training site each year for eight 3rd year medical students from UNECOM. Since 2012, BMC has also offered an Osteopathic Neuromusculoskeletal Medicine (ONMM3) post-graduate program, for specialty-level training in ONMM following an Internal Medicine or other primary care residency program.
Osteopathic Focus Track within Internal Medicine:
With the AOA-ACGME merger in 2020, Osteopathic residents in our program can now opt-in (fully optional) to participate in continued osteopathic training (our “Osteopathic Track”) during their Preliminary or Categorical Internal Medicine Training. This Osteopathic Track is a fully-accredited Osteopathic Recognition program by the ACGME and allows graduates to move forward with “Distinction of Advanced Osteopathic Training” as conferred by the AOA. This Osteopathic Track is in-addition to all typical educational elements for Internal Medicine, and consists of:
- Participation in a weekly osteopathic didactic series
- Participation in our monthly Osteopathic Grand Rounds comprised of osteopathic journal club, anatomy and philosophy readings, as well as both lecture and hands-on lab to learn and practice various osteopathic techniques.
- Participation in our OMM continuity clinic where residents see and treat patients under the supervision of an ONMM trained preceptor.
- Participation in our Osteopathic Manipulative Medicine consult service for hospitalized patients
- Enrollment for a yearly OMM-specific knowledge assessment exam (the CORTEX exam)
- Attendance at a regional Osteopathic teaching conference (the ASSSG)
Contact:
Stephen Kisiel, DO
Program Director, Osteopathic Focus Track
Berkshire Medical Center
skisiel@bhs1.org
Lisa Blay
Program Coordinator, Osteopathic Focus Track
Phone: 413-447-2839
Fax: 413-447-2088
lblay@bhs1.org

Internal Medicine FAQs
01
What type of Visa is offered?
We sponsor J-1 Visas for Preliminary Year Residents, and H1B Visas for Categorical Residents.
02
How many attempts to pass the US Medical License Exam steps are accepted?
Applications are neither accepted nor rejected for interview based on a single factor. Applications are evaluated based on multiple criteria including but not limited to: work experience, letters of reference, prior training, diversity of life experiences, performance in medical school, test scores, etc.
03
How long since graduating from Medical School is acceptable?
We do not have a set cutoff graduation date
04
How many recommendation letters are required?
Three (3) letters are required.
05
Do recommendation letters have to be from institutions/physicians within the United States?
No, your recommendation letters do not have to come from locations in the United States.
06
When is your application deadline?
The deadline to apply to our program is December 1.
07
When do you schedule interviews?
Interviews are scheduled from mid-October through January and are virtual.
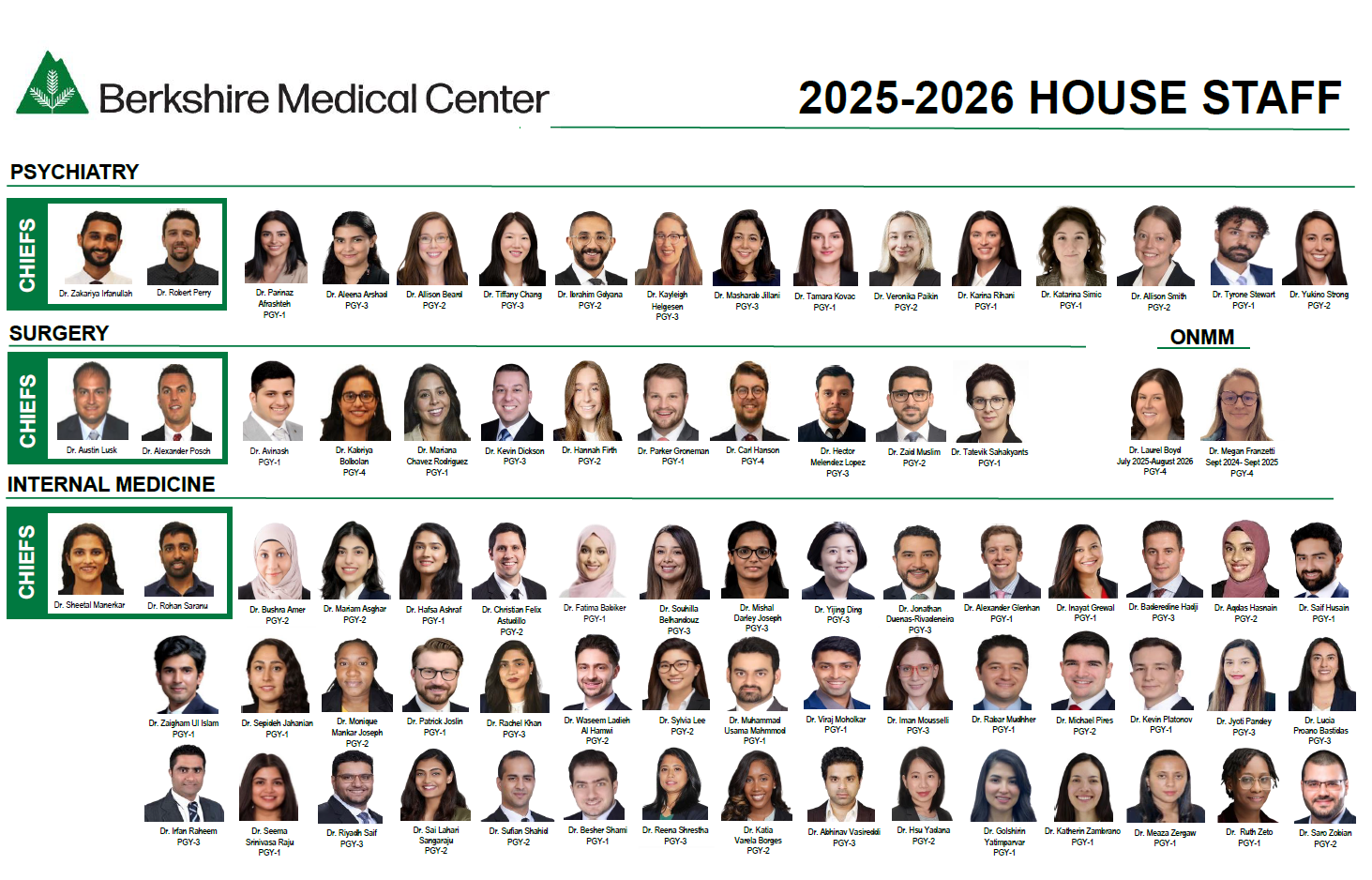
Meet Our Team
Our Residents
Our alumni are successful in achieving high quality competitive fellowships and outstanding positions as internists either in hospital or outpatient practices throughout the United States. We have included a sampling of positions taken by recent graduates of the BMC Internal Medicine Residency below.
Fellowship Positions:
- Cardiology: Baystate Medical Center
- Cardiology: University of Arizona
- Critical Care: Mercy Medical Center
- Critical Care: Geisinger Medical Center
- Endocrinology: Boston University
- Endocrinology: Marshall University
- Endocrinology: SUNY Upstate Medical Center
- Gastroenterology: Mountain Vista Medical Center
- Hematology Oncology: St Elizabeth’s Medical Center
- Hematology-Oncology: University of Vermont Medical Center
- Hematology Oncology: Virginia Commonwealth University Medical Center
- Hematology Oncology: Dartmouth Medical Center
- Infectious Disease: Baystate Medical Center
- Infectious Disease: Tufts Medical Center
- Infectious Disease: Yale Medical Center
- Nephrology: University of Massachusetts
- Nephrology: Massachusetts General Hospital
- Nephrology: Allegheny Medical Center
- Nephrology: New York University
- Nephrology: Washington University Medical Center
- Nephrology/Critical Care: Yale University Medical Center
- Pulmonary/Critical Care: St Elizabeth’s Medical Center
- Pulmonary/Critical Care: University of South Alabama
- Pulmonary/Critical Care: Yale University/Bridgeport Medical Center
- Pulmonary/Critical Care: University of Oklahoma Medical Center
- Pulmonary/Critical Care: Vassar Brothers Medical Center
- Rheumatology: Albany Medical Center
- Rheumatology: University of New Mexico
- Sleep Medicine: University of Minnesota Medical Center
Hospitalist Positions – nationwide, including local centers such as:
- Baystate Medical Center, Massachusetts
- Berkshire Medical Center, Massachusetts
- Brown University Hospital, Rhode Island
- Cape Cod Hospital, Massachusetts
- Metrowest Medical Center, Massachusetts
- St Peter’s Hospital, Albany, NY
- St Vincent’s Hospital, Massachusetts
- UMass Medical Center, Massachusetts
Primary Care Positions:
- California
- Florida
- Massachusetts
- New York
- North Carolina
- Ohio
- Rhode Island
- South Carolina
- Texas
- Washington
Essential Functions
Residents in our program work & learn in a variety of settings and clinical roles. Essential job functions of a resident physician’s role in our residency program include the ability without an intermediary to:
- Take a history and perform a physical examination of patients.
- Communicate with patients and staff, verbally and otherwise in a manner that exhibits good professional judgment and is appropriate for the professional setting.
- Read charts, monitors, and other sources of clinical information.
- Complete appropriate medical records and documents and plans according to protocol and in a complete and timely manner.
- Possess sufficient sensory and motor function to elicit information from patients by palpation, auscultation, percussion and other diagnostic maneuvers.
- Be able to execute motor movements reasonably required to provide general care and emergency treatment to patients.
- Perform all job functions while dressed in protective clothing required for clinical duties, including tolerating a mask, gown, and gloves.
- Move throughout the Medical Center to address routine and emergent patient care issues and to attend required educational programs.
- Work shifts of varying lengths and schedules including daytime, evening, & overnight clinical shifts.
- Fulfill backup and on-call duties as scheduled.
- Provide care at all clinical sites, including Berkshire Medical Center, our Ambulatory clinic, and other affiliated practices of BMC (the Cancer Center, etc..).
- Utilize a computer for medical record review, documentation, decision support, research, and education in an efficient and timely fashion.
- Possess the emotional health required for full use of their intellectual abilities, the exercise of good judgment and the prompt completion of all responsibilities attendant to the diagnosis and care of patients.
- Have the emotional maturity to self-assess, know own limitations and seek advice or counseling in situations that might impair own learning or performance in the care of patients, and to proactively seek appropriate treatment.